This post was updated Jan. 28 at 4:32 p.m.
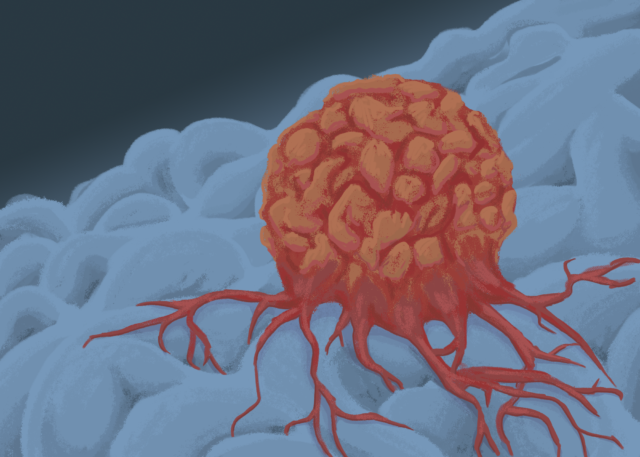
UCLA researchers developed a new cancer treatment that could be useful for targeting solid tumors.
In the study, the researchers said they developed a biodegradable scaffold that is implanted near solid tumors to modulate the immune system’s response to cancer and modify the tumor microenvironment. Cancer cells modify the tumor microenvironment to allow them to rapidly proliferate and disable the immune system to prevent it from destroying the tumor, according to an article in Cell Proliferation.
According to an article in the scientific journal Frontiers in Immunology, one of the ways it does this is by exhausting cytotoxic T-cells, which are immune cells that kill cancer cells.
Cancer cells can also saturate the tumor microenvironment with regulatory T-cells – immune cells that can suppress the immune response – according to an article in Frontiers in Immunology.
Dr. Manish Butte, a professor in the department of pediatrics and a corresponding author, said they hoped the study could advance treatment for solid tumors.
“So far, many of the immune therapies have had a hard time with solid tumors,” Butte said. “Coming up with a new way of helping the immune system fight solid tumors was one of our goals.”
Therefore, the researchers wanted to create a treatment that would activate the immune cells close to the tumor, said Dr. Negin Majedi, an alumnus of the doctoral program in bioengineering and co-author of the study.
“(The idea was to have) a structure that could be placed beside a solid tumor and act as a training boot camp for the immune cells,” Majedi said.
They decided to create a structure that mimics lymph nodes, where the immune cells are normally activated, to optimize the activation of the immune cells, Majedi said.
The scaffold is pre-loaded with substances that recruit and activate immune cells before it is surgically implanted near the tumor, where these substances are released.
Initially, the researchers used the scaffolds to target a range of immune cells, but found that optimizing the scaffold to focus on eliminating regulatory T-cells was extremely effective, Butte said.
“No other biomaterial, no paper or no technology anywhere published can get rid of regulatory T-cells inside of tumors,” he added.
The researchers tested the scaffold by implanting it into mice with breast cancer and mice with melanoma, according to the study. They found a significant reduction in the number of regulatory T-cells and an increase in the effectiveness of the cytotoxic T-cells in the mice, which reduced tumor growth and the spread of cancer cells.
The scaffold also prevented the recurrence of cancer, signaling they had effectively trained the immune system to have a long-term memory of cancer, Majedi said. The mice that survived the primary tumor were injected with the tumor again to see whether it would grow back, she said, adding that the tumor did not grow back in any of the mice.
Additionally, unlike many cancer treatments which can adversely affect the whole body, scaffolds locally modulate immune activities, according to the study.
This scaffold could potentially be combined with other cancer treatments, Majedi said. One possible avenue is to use the scaffold to deliver chimeric antigen receptor CAR T-cell therapy, a type of cancer treatment in which a patient’s T-cells are engineered to target cancer cells, according to the National Institutes of Health. It has only been effective in treating liquid cancers so far, according to the study.
“One idea would be to actually load those engineered CAR Ts and place them inside the solid tumor,” Majedi said. “It could be the perfect kind of cargo for carrying those engineered CAR Ts.”
The researchers tested the delivery of CAR T-cell therapy with delivery of engineered T-cells via the immunoactive scaffold. This led to prolonged survival in mice with melanoma compared to when only the immunoactive scaffold was used.
Yvonne Chen, an expert on CAR T-cell therapy and associate professor of microbiology, immunology and molecular genetics and chemical and biomolecular engineering, said she agrees there could be a benefit in using CAR T-cell therapy with the scaffold.
“By encasing CAR T-cells in the scaffold and physically placing it near the tumor, one could potentially facilitate T-cell trafficking to the tumor mass,” Chen said.
However, Chen noted that for this scaffold to work, the tumor must be located in an area accessible by surgical procedures so the gel can be implanted nearby.
A future route to refine this technology is to make it injectable so it is easier to access the tumors that can’t be reached by surgery, Majedi said. The ultimate plan going forward is to have this scaffold tested so it can become available to cancer patients.
“We want to try to treat humans with solid tumors,” Butte said. “We’re going to go after ones where there are few, if any, existing therapies. The first one on the list is triple-negative breast cancer.”


Comments are closed.